One morning in April, I woke up unusually groggy. I brushed it off as a bad night’s sleep, skipped my usual Pilates class, and pushed through the day. But by 10 a.m., a wave of crushing fatigue knocked me flat. That same exhaustion hit the next day. And the day after. Before long, I was sleeping over 12 hours a day and could barely stand for more than a few minutes at a time.
Frustrating weeks of bloodwork, imaging, and specialist visits followed. Every test came back “normal” yet I felt anything but. Perplexed, I turned to my new friend: Dr. Perplexity. I plugged my symptoms, labs, and history into Deep Research Mode and asked for the most probable diagnoses.
It flagged something unexpected: small intestinal bacterial overgrowth. Neither I nor my doctors considered that my gut could be the culprit. But sure enough, a gastroenterologist confirmed the diagnosis, and began treatment that finally brought relief.
I share this story not to highlight the incredible potential of AI in health care (though I absolutely believe it), but because the gut was the last place my doctors and I thought to look, since my symptoms were largely cognitive.
Many Americans feel uninformed about their gut health. When an Ipsos poll quizzed over 1,000 U.S. adults about the gut, 85% received a failing grade and none got an A. Below are a few questions from the quiz; see how you fare!
True or False?
True
True
False
True
True
True
True
True
If you didn’t do well, you’re not alone. But ignorance is dangerous, given the pivotal role of our gut in our overall health.
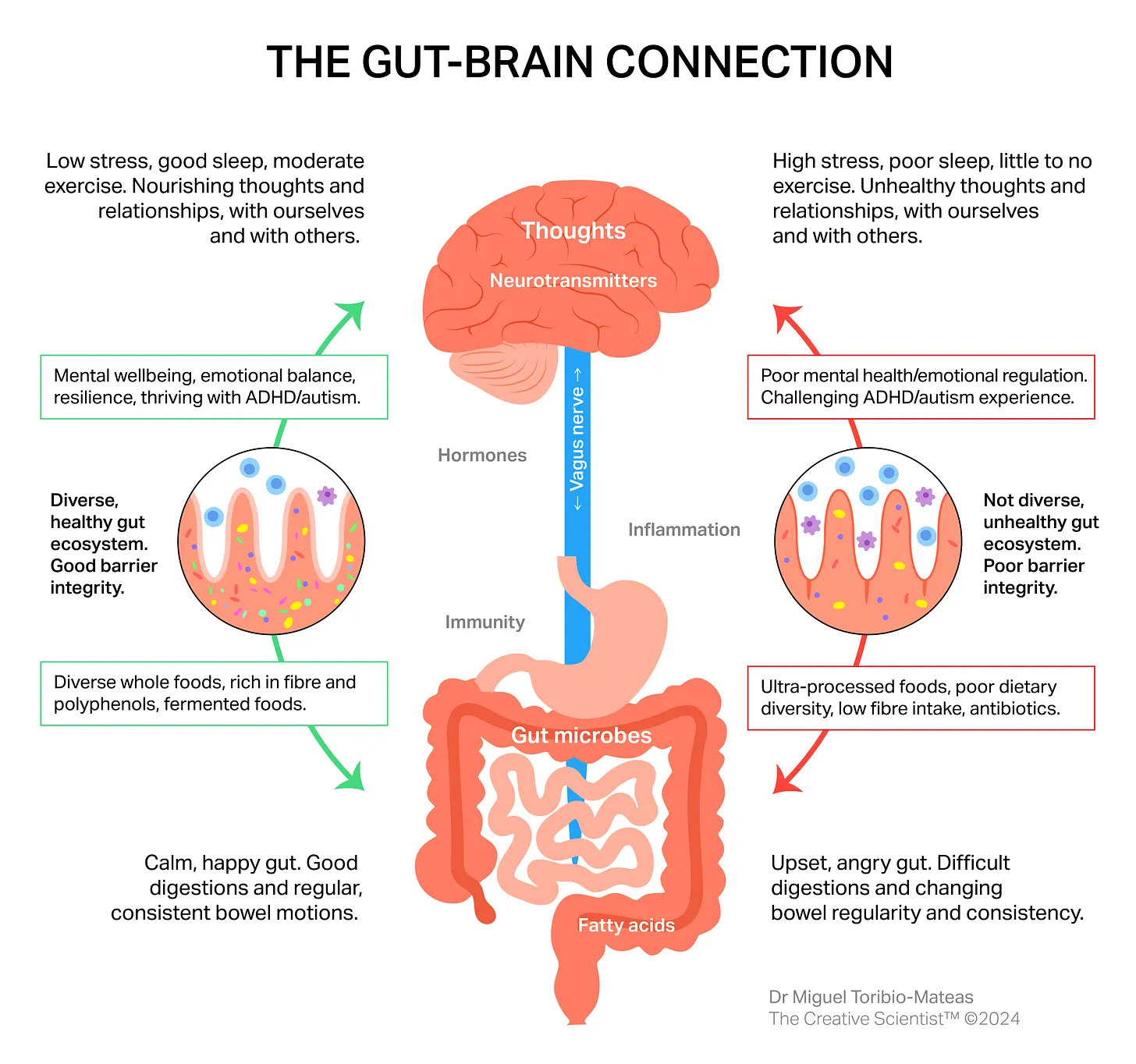
Through its microbiome and interactions with other organs, the gut is fundamental to our health across multiple body systems. It is responsible for digestion and nutrition absorption, the production of essential compounds such as B12, disease prevention and detoxification, and influences mental and cognitive functions. As the body’s largest immune organ, the gut contains 80% of immune cells and is central to our immune system regulation.
More Than a Gut Feeling
A balanced gut correlates with improved immunity, nutrient absorption, blood glucose and lipid balance, and energy metabolism, while producing essential vitamins.
By contrast, an imbalanced gut microbiome often leads to health issues. A comprehensive study conducted at Harvard, Brigham and Women’s, and the Broad Institute found a relationship between changes in the gut microbiome and Type 2 Diabetes. Links have also been established between an imbalanced gut microbiome and obesity and depression. Introducing “healthy” gut bacteria into mice reduced anxious behaviors, while fecal transplants from humans with depression increased depression and anxiety-like behaviors in mice.
Scientists call the gut as our “second brain.” The enteric nervous system is the neural network in the gastrointestinal (GI) tract and controls its digestive functions. With more than 500 million neurons, this system is the most complex neural network outside our brain, and can operate somewhat independently. The nerve connecting our enteric nervous system to our brain conveys important information about our gut condition to our brain, and motor signals from our brain to our gut.
Despite its importance, gut health is not well understood or practiced in traditional health care. In a survey of physicians across 60 countries, just 59% said they had average or below average knowledge of the gut microbiome. Only 3% reported using microbiome composition analysis regularly, and 63% said they never use it. Many cited a lack of reference values, reimbursement, applications in clinical practice, and difficulty interpreting the results as the reasons.
This has real implications. In a survey of over 500 primary care providers across the U.S. and Europe, 90% agree the causes of irritable bowel syndrome (IBS) are poorly understood and 80% say IBS is underdiagnosed in primary care practice.
The Cost and Impact Opportunity
While traditional healthcare is catching up, consumers are eager to better understand the role their gut plays in their health. On TikTok, #guttok content now has over 7 billion views and #gutmicrobiome gets over 730,000 views every week.
As the science on gut health improves and consumers get smarter, there is a massive opportunity to modernize gut-based holistic health. Gastrointestinal diseases impact 70 million Americans each year (twice as many as those living with diabetes). Direct healthcare costs for GI diseases are estimated at $136 billion annually, more than heart disease ($113 billion) and mental health disorders ($99 billion). Digestive diseases make up nearly 20% of all surgeries in America. Every year there are roughly over 50 million ambulatory visits related to GI issues, three million hospital admissions, and 266,000 new cases of GI-related cancer diagnosis. Colorectal cancer is now the third leading cause of cancer death in both men and women.
The impact extends beyond health and digestive problems. On average, individuals with IBS miss 13 days of work or school per year, compared to five days for those without. Given the connection between the gut and the brain, 25-30% of IBS patients suffer from depression or anxiety, a rate 6 times higher than healthy peers.
The economic toll of gastrointestinal issues on healthcare systems is hard to ignore, and consumers are desperate for solutions. The global market for digestive health products was $51 billion in 2023 and is projected to reach $58 billion by 2030. Most importantly, the current impact on patient health and quality of life is unacceptable.
Gut Health: Where We’re Investing
At Reach, we love the intersection of emerging science, latent consumer demand, and massive opportunity for impact. Below are a few areas in the gut health market we are excited to invest in.
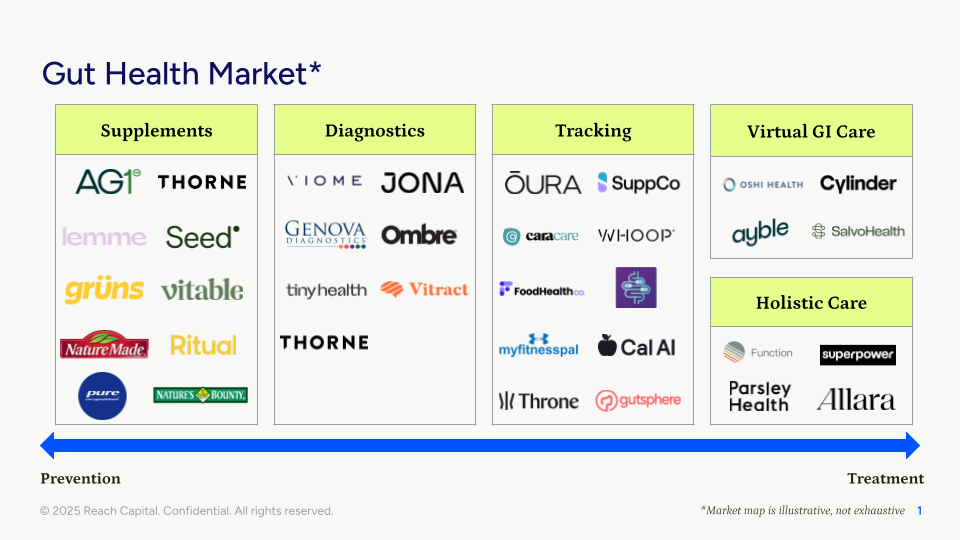
1. New diagnostics that provide better data for personalized recommendations. Historically, it has been difficult to determine what “good” gut health is given the diversity of gut microbiomes across different geographies and demographics. But there is an opportunity to create more personalized diagnostic tools to drive care and make data actionable for the consumer.
More precision is essential. Women, for instance, empty food from their stomach slower than men, which may be why they experience nausea and bloating more frequently. They are more likely to use pain relievers (for headaches, period cramps, etc.), which can create stomach inflammation. Women have slower gallbladder emptying than men and so are twice as likely to develop gallstones, particularly during pregnancy due to unique hormones.
These examples highlight why there isn’t a “one size fits all” solution. But science is advancing. Researchers at Mayo Clinic developed a computational tool that analyzes the gut microbiome and reached at least 80% accuracy in differentiating healthy individuals from those with diseases. It was built by analyzing stool gut microbiome profiles across more than 8,000 samples from different demographic groups, and diseases from 54 published studies across 26 countries and six continents, making it one of the largest datasets of its kind. While the tool is not yet intended to diagnose specific diseases, it can help examine an individual’s gut health trends and recommend dietary or lifestyle modifications.
Companies like Viome, Thorne, and Tiny Health have popularized the concept of at-home gut health tests. That said, more work is needed to better personalize these exams, make the data actionable for consumers, and connect it to their overall health profile to drive better outcomes. We like the approach companies like Throne are taking to provide data like bowel movements that is critical for gut health but historically difficult to track over time (WHOOP for your poop!).
2. Enabling all clinicians to integrate gut health into their care. The best way to engage the most patients is through their existing healthcare experiences, so embedding gut health into a physician’s flow of work is critical. But as the aforementioned surveys show, a lack of knowledge among doctors is a major barrier.
We are interested in solutions embedded in existing tools (i.e. EHRs) used by clinicians and which can make personalized recommendations to help manage patient care. These will look different based on the clinician (primary care provider, gynecologist, behavioral health therapist, etc.) to provide the best form of holistic care. Ideally, these tools can get a full cycle of information from diagnosis to resolution to build a large dataset for future research-based care.
As someone recently diagnosed with a gut-related issue, my “solution” was a prescription for two different antibiotics and a printout of a “low FODMAP diet” to follow. There was no acknowledgment of my specific gut microbiome or suggestions on how to rebuild my gut after the blunt antibiotic treatment. There is a lot of room for improvement. We are starting to see testing companies like Jona and Vitract build for the clinician, but adoption is still early. There are also holistic health-specific EHRs like Vibrant emerging that enable clinicians to provide more personalized care across the board, including the introduction of gut health.
3. Consumer tracking tools that incorporate diet, lifestyle data, and supplements and can close the gap between data and action. My colleague Caoimhe’s latest piece on consumer-centric healthcare shares our thesis on the need to connect fragmented consumer health data to power hyper-personalized care at scale. We expect gut microbiome data to be a big part of the mix, and how lifestyle, diet, and supplements may impact the gut and overall health.
Anecdotally, I currently track my food and macros on Cal AI, my health data on my WHOOP, supplements on Supp, and then have my healthcare data across a range of different EHRs. None of this information, however, is “speaking” to one another, thus missing out on a treasure trove of critical information and helpful insights.
We are eager to invest in solutions that help to bring gut health to the forefront of modern healthcare. If that sounds like what you’re building, please reach out to jomayra@reachcapital.com!